Abstract
Background While formerly known as idiopathic thrombocytopenic purpura, the mechanism of ITP is now well understood as immune-mediated. Based on etiology, ITP is categorized as primary and secondary. Whereas secondary ITP is associated with an underlying condition, diagnosis of primary ITP is based on excluding other causes of isolated thrombocytopenia. The clinical course can be variable with approximately 80% of patients experiencing recurrence after first-line therapy (Ghanima W et al, Blood, 2021). Chronic inflammation and immune stimulation have been linked to the development of a variety of autoimmune conditions, including ITP. The production of "adipokines" in obesity induces an inflammatory state that triggers and worsens the outcomes of various immune-mediated conditions (Versini M et al. Autoimmune Rev, 2014). Studies evaluating obesity and ITP are extremely scarce, with only one reported case series which included three obese pediatric patients (Hanafy E et al. Ochsner J, 2017).
Obesity has become a growing public health problem in the United States and can cause serious health and financial consequences. Patients diagnosed with ITP also experience substantial economic burdens and affected quality of life (Derek W et al. Hematology, 2019; Cooper N et al. Am J Hematol, 2021). We conducted a retrospective study aiming to investigate the relationship between ITP and obesity.
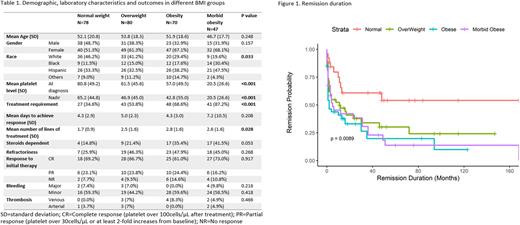
Method Using the keyword "immune thrombocytopenia," we extracted patients over 18 years old between May 2012 to May 2022 from the electronic medical record systems of Montefiore Medical Center with data mining software. Secondary ITP such as active or chronic viral infection, H pylori infection, connective tissue disorder, positive rheumatologic serology, lymphoproliferative disorder, medication and pregnancy-associated ITP were excluded from the study. Patients were categorized into four groups based on their BMI at diagnosis: regular weight (< 25), overweight (25 - 29.9), obesity (30 - 40 or 35 with complications) and morbidly obesity (>40 or 35 with complications). Baseline demographic, laboratory characteristics and outcomes were compared between groups. The ANOVA test was used to compare the continuous variables and the Chi-Square test was used for categorical variables. The overall response duration to initial treatment was calculated by Kaplan-Meier model.
Result A total of 759 patients with ITP were identified, after excluding secondary ITP and insufficient data, 275 patients with primary ITP were enrolled. There is no difference in gender and age at diagnosis between the four groups. There was a higher proportion of minorities among patients with higher BMI (p=0.033). Patients with higher BMI had significantly lower platelet levels both at diagnosis (mean platelet level 80.8, 61.5, 57.0, 20.5 for regular, overweight, obesity and morbid obesity, respectively, p<0.001)and nadir during the course (mean platelet level 65.2, 46.9, 42.8, 20.5 for regular, overweight, obesity and morbid obesity, respectively (Table 1). Patients with higher BMI were more likely to require treatment(p<0.001). Among the patients who required therapy, there was a trend for association between obesity and steroid dependency (p=0.053). Obesity was also associated with the need for more lines of treatment (p=0.028). Among the patients who received corticosteroids as first-line therapy, non-obese patients had a longer duration of remission compared to the obese patient (median response duration, not reached vs. 11 months, 2 months, 5 months, for regular vs. overweight, obese, morbid obese respectively p=0.0089) (Figure 1). There is no difference in the level of response, time to response, refractoriness, bleeding and thrombotic complications among the groups (Table1).
Conclusion This is the first retrospective study illustrating the relationship between ITP and obesity. Obese patients had overall lower platelet levels, were more likely to require therapy, were more steroids dependent and needed more lines of treatment. Obese patients who responded to therapy had a shorter remission duration than non-obese patients. Our study suggested that obesity is an adverse risk factor for ITP. Our data demonstrate obesity is associated with adverse ITP outcomes and weight loss modality could potentially provide synergy with ITP directed therapy.
Disclosures
Murakhovskaya:Alexion: Research Funding; Annexon: Research Funding; Kezar: Research Funding; Rigel: Consultancy, Research Funding; Sanofi: Consultancy, Research Funding; Incyte: Research Funding; Novartis: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal